The Fittest Doc Answers: Are You at Risk for COVID
♦
Special guest Dr. Nick, MD—the "Fittest Doc"—sits down with Aaron Hinde D.C. (president and co-founder of LIFEAID) to debunk some common myths about the Coronavirus. The two doctors also share important facts, health tips and suggestions to stay healthy and protect our community during this time. Watch the interview now to learn more about COVID-19, including how practicing gratitude & mediation are beneficial to help boost your immune system! (35:45)
WATCH THE VIDEO HERE: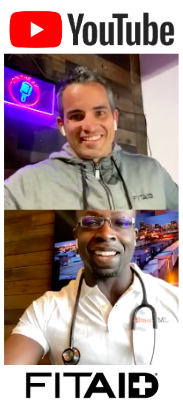
Full transcription of the audio recording from the interview with Dr. Nick, MD, and the co-founder of LIFEAID Aaron Hinde, on Wednesday, March 11, 2020.
Aaron Hinde: Hey, doc, how's it going?
Dr. Nick: (0:01) Hello. Hi, how are you, Aaron?
Aaron Hinde: (00:03) Looking good, doing well. Thank you. Thanks for taking the time today. And thank you, everyone, for joining. We've got an interesting conversation with Dr. Nick from SteadyMD, @thefittestdoc on Instagram, and Dr. Nick and I have had a chance to hang out together, and I can tell everyone on the line right now, he absolutely is the fittest doc as you can see from the image there on the phone. So what did you just squat the other day? You almost did a 500-pound squat, right?
Dr. Nick: (00:35) Yeah, 485 successfully, and 500-pound fail.
Aaron Hinde: (00:39) Oh, man. Congrats. That's amazing. That's amazing. Well, I can speak from experience, being in the healthcare field for 10 years myself and meeting hundreds of docs, you definitely are the fittest doc. So keep up the good work.
Dr. Nick: (00:53) I'm pretty sure Julie Foucher is, but this is a Coronavirus talk so--
Aaron Hinde: (00:58) We'll give you the fittest male doc. How about that?
Dr. Nick: (01:00) Okay.
Aaron Hinde: (01:02) So today, we're going to talk about something very topical, very much in the media. Everybody's talking about it; everybody's very concerned about it; which is the Coronavirus. So we wanted to get an authority figure like yourself, somebody educated in medicine to kind of set the record straight. There's just a lot of fear mongering going on right now in the media and misinformation being spread. So wanted to set the record straight. So why don't you just tell everybody, what is a coronavirus? How does it spread? Is there something we should be afraid of here?
Dr. Nick: (01:40) So Aaron, first of all, thank you for giving me the opportunity to speak on this. But essentially, coronaviruses are actually pretty common human viral infections. They were initially identified in the 1960s, and they commonly spread person-to-person. There are, in total, seven coronaviruses that can infect people. Amongst them, there are actually two common what are known as alpha coronaviruses, two common what are known as beta coronaviruses. These common variants are among the viral infections that cause the common cold. Additionally, there are also MERS Coronavirus, SARS, that, you know, everybody heard about a couple years back. That is a coronavirus variant. And now, this coronavirus, also known as COVID-19, is also known as SARS Coronavirus too. So this is what's called a novel coronavirus, and that essentially implies that is a coronavirus that, in the past, was not known to infect human beings. And as I stated earlier, it's currently known as, specifically, COVID-19. So these last three, MERS, SARS, and COVID-19, are notable because they were initially relegated strictly to animals. They subsequently evolved and are now capable of making people sick.
Aaron Hinde: (03:28) So they made the jump, so to speak, from animals to humans.
Dr. Nick: (03:32) Absolutely.
Aaron Hinde: (03:34) Similar to how we anticipate AIDS first started in an animal population and--
Dr. Nick: (03:39) Sure, sure. Absolutely. So in terms of spread kind of between people and how that happens-- So it is currently thought that this is a primarily respiratory droplets exposure spread virus. So it may be possible, yes, that a person can get COVID-19 by touching a surface or an object that the virus has been on and then touching their mouth, touching their nose, touching their eyes. But currently, it is not thought that that is the main way that the virus spreads. Also, there is currently no evidence to support the suspicion that COVID-19 can be spread through transmission of food. So I know that some people have concerns about certain-- whether it's items coming in from China or other places exposed to COVID-19 or food, people seem to have a concern about that. And insofar as we've currently seen, that is not a concern. There's nothing, essentially, as of right now, to support that from an evidence-based standpoint.
Aaron Hinde: (05:01) No, I appreciate you clearing that up. So what type of symptoms would someone expect to get? How long is the incubation period? What symptoms would develop? And how could you mitigate the spread of COVID-19?
Dr. Nick: (05:19) So currently, the incubation period - which I know a lot of people have heard so far, for COVID-19 is thought to be 14 days- oftentimes, it can actually-- symptomatically, people can start showing symptoms within three to six days in general. At least for that two-week period, at least for 14 days right now, it's thought to be the incubation period. Symptomatically, when patients do start to experience symptoms, actually, that implies that all patients experience symptoms, and that's not entirely true. So essentially, as of right now, the range of infected patients is all the way asymptomatic - no symptoms at all - to fever, to kind of symptoms of an acute respiratory illness, including but not limited to cough, difficulty breathing, to myalgias, which are essentially--
Aaron Hinde: (06:23) Muscle pains.
Dr. Nick: (06:23) --tenderness and kind of-- Exactly, muscle pain, to fatigue, to what's called an ILI, and influenza-like illness, and at its most severe, currently, COVID-19 has presented in a small but important population with severe pneumonia, with kind of respiratory failure and, in some people, with septic shock. So it has a wide variety of presentations, and given the current death rate, the current death toll, rather, of this, it can absolutely be presumed that a number of individuals have this asymptomatically. There have already been a number of cases of recoveries all around the world, so yeah.
Aaron Hinde: (07:17) There was one estimation that the reason that kids are not contracting this symptomatically, say, is because they've already got some form of the coronavirus or one of the seven type of mutations that you discussed earlier in school, and so they already have some built-up immunity. Is there any truth to that?
Dr. Nick: (07:40) Yeah, you know, that's an interesting thought. In terms of what is known from the CDC, in terms of what is known by the governing health bodies, there's currently no known data specifically regarding-- as such, I can't comment on that with any amount of certainty.
Aaron Hinde: (08:02) Sure, sure. Now, I have read from the WHO that the mortality rate, the death rate with this is significantly higher than, say influenza or the common-- People of the common cold, as high as three and a half percent. Now, when I read that, my first thought was, "Well, they're taking known cases, meaning you have to be symptomatic enough to go in and get treatment, and then three and a half percent of those people are dying." But we've also read - and please clarify this - that up to 80% will be mildly symptomatic or asymptomatic, so much so that they're not even going to seek medical treatment. So it appears to me that, when this all plays out, that three and a half percent is going to be way on the high side, and this could easily come in well under 1% or even a tenth of a percent because of the number of asymptomatic people that will never seek treatment as a result.
Dr. Nick: (08:57) Yeah, Aaron, so what you're speaking on there is what's called a case fatality rate. So originally, when this first hit, the data coming out of China, coming out of approximately 70,000 in China, estimated that the case fatality rate was 2.5%. However, just this week, the WHO, the World Health Organization, released their own figures and their own numbers, saying that the number was 3.4%. So they actually-- I mean, the percentage according to them was actually a little bit higher. And that number was computed looking at the number of confirmed cases and then case fatality within that. However, as you noted - and I think that's a very notable observation that you made - there are likely thousands and thousands of people who are infected, and as I noted earlier, who are infected and asymptomatic. And if you look at the map here, the numerator and the denominator of figuring out the case fatality rate, people who are walking around infected and asymptomatic, and furthermore, those who stay asymptomatic over the course of their infection and completely recover from it? Those people, if they were counted, would change the denominator--
Aaron Hinde: (10:22) Significantly. Significantly.
Dr. Nick: (10:23) Absolutely. So as such, I think that, essentially, as more testing kits become available worldwide and they become more widespread, we will be able to accurately calculate how many people are infected and the case fatality rate. But essentially, if you want to look at it compared to other infections, flu is estimated at a case fatality rate of .06 to .1%, kind of depending on the year and the impact of the flu for that year. SARS was calculated at about 10%, and MERS Coronavirus was calculated at about 30, 34%.
Aaron Hinde: (11:05) Gotcha. Okay. That's good information. And just to put things in perspective, I read the 2017-2018 flu season, about 35 million Americans got some form of influenza in that flu season. We're talking about, worldwide, so far, 110,000 cases of Coronavirus worldwide that have killed approximately 3,500 people as of this morning. And put that in more perspective: 26,000 die every day in this country from-- worldwide - I'm sorry - from cancer; almost 50,000 from cardiovascular disease. 3,000 people die a day from mosquito bites, believe it or not.
Dr. Nick: (11:47) Wow. Did not know that.
Aaron Hinde: (11:49) Yeah. Okay, so let's talk about your immune system. We had a question I saw come through: does seasonality come into effect here? As things warm up, we always see the common cold, influenza cases go down, I think because we're getting more vitamin D exposure. But would love to have your thoughts on that. Would you expect to see some seasonal adjustment here?
Dr. Nick: (12:13) You know, that is another thing that I think would be irresponsible any healthcare practitioner to comment as of now, because insofar as I know, Aaron, there is no absolute data speaking on COVID-19 and its uniqueness. As I stated - right? - this is a novel coronavirus. So given that we simply don't have enough data to state with certainty that this is something that, over the summer, will decrease.
Aaron Hinde: (12:46) Because there are so many people that are asymptomatic or minimally symptomatic that have a possibility to contract this, what is the difference between the symptomatic group and the asymptomatic or minimally symptomatic group? In your estimation.
Dr. Nick: (13:02) How so?
Aaron Hinde: (13:03) I'm just saying, why would I get severely sick and somebody else not be symptomatic at all? Does that have to do with how well our immune system is functioning or--?
Dr. Nick: (13:15) I understand. So one could argue that that absolutely plays a part. With the data that has come out of China thus far, rather, there is absolutely a male predominance. There seems to be a male predominance with this, though I will disclose that that was likely biased by the fact that men in that cohort in China were very commonly smokers and had chronic lung disease. But otherwise, the people who seem to be hit the hardest, at least from the data coming from China, are immunocompromised. So those who are post-transplant, have cancer, even something like diabetes and the elderly who chronically live in a state of immunocompromised compared to the younger and healthy. Paradoxically, at least for now, insofar as I know, there have not been any diagnosed cases in children younger than nine years old. So it seems that, at least for now, from what I've observed, children seem to be relatively spared.
Aaron Hinde: (14:34) Great, that's good to hear. What can we do to boost our immune system? And there's a lot of-- Let's start with exercise. There's differences in opinion. "Should I go to the gym? Should I not go to the gym? Should I do low-impact, easy exercise, or should I go more CrossFit style, high impact? High intensity, I should say."
Dr. Nick: (14:59) So exercise, I think-- From the research that I've seen, exercise is no different on the body than any other stressor. So I think a better question here is how does stress affect the immune system? And how I would answer that is that it very much depends. So transient stressors, such as those associated with work, with family, or even exercise, absolutely have been shown to be associated with a bolstering and strengthening of the immune system. Unfortunately, more chronic, consistent stressors, those that are not remitting in nature such as a chronically stressful job or home life or even persistent non-transient states of anxiety, especially those of the untreated type, tend to absolutely cause a persistent inflammatory state physiologically, and with that, a persistent depression of our own ability to fight off infection.
Aaron Hinde: (16:10) So those people that are kind of constantly in that fight-or-flight mode, you want to get out of that. I know in my job--
Dr. Nick: (16:16) Absolutely.
Aaron Hinde: (16:16) --obviously here at LIFEAID can be pretty hectic on a daily basis. And as a part of my morning routine, being very clean with my diet, practicing breath work, meditation, making sure I get really good sleep, staying hydrated right when I wake up in the morning and throughout the day. Do you practice any of that? How does that tie in, do you think, to your overall immune function?
Dr. Nick: (16:45) Yeah, so I think that those type of activities absolutely benefit immunity. Essentially, those are what I like to call mindfulness techniques, right? And they have absolutely been shown-- Kind of one of my favorites with my patients is cognate immunity and CBT, cognitive behavioral therapy, has absolutely been established for quite some time now in that it can positively affect mood with that, and essentially cause a lessening of mental stress and anxiety. And then, obviously, that will obviously positively affect our immune system. So kind of personally, what I try and do for myself is practice gratitude. I have a gratitude journal that I try to write in when I wake up in the morning. And something that I've been getting into more recently that I used to be into in high school and then fell out of it, was meditation. And I definitely think that's something that's definitely beneficial for us in the long run.
Aaron Hinde: (17:54) It's funny: we're discussing ways to reduce chronic stress and therefore boost your immune function, yet in most-- And a lot of people know, I don't have a television. I don't listen to typical radio, and just don't subject myself to newspapers and all that. So I'm not into the hype and hysteria that is being kind of forced on people right now. But all of that is very fear-driven, creating this chronic stress response, which is the exact opposite of what we need to be doing for our immune system. It's very ironic to me.
Dr. Nick: (18:33) That's paradoxical.
Aaron Hinde: (18:34) It's very paradoxical.
Dr. Nick: (18:35) Absolutely.
Aaron Hinde: (18:37) Let's get into supplementation. Do you take any specific supplements yourself for immunity? And do you think vitamin C, vitamin D, echinacea, these types of things are worthwhile?
Dr. Nick: (18:51) So personally, Aaron, I do not. I do not take any supplements, simply because I eat a whole foods-based diet. As you stated earlier, you're very good about your diet. I think that, when you are eating a whole foods-based diet, it becomes redundant. Now, let's back up: I'm not saying that, if you take certain supplements while eating a whole foods-based diet, that there's anything bad with that. In fact, essentially, your kidneys will excrete that. So at most, taking these supplements could be wasteful because you could quite literally pee them out. You could excrete them. But I think that, essentially, if you're on a whole foods-based diet, you don't need that. Now, otherwise, there are kind of some non-traditional therapies used for the common cold including echinacea, vitamin C, zinc. For those three that I just mentioned, there is really no solid evidence that either of those effectively treat the common cold. However, there absolutely is some data that show that a significant decrease in illness duration can be had if you are taking vitamin C before the onset of symptoms.
Aaron Hinde: (20:17) I've been on a diet ever since this thing hit of about five IMMUNITYAIDs a day--and after the fourth one, my pee goes totally bright yellow. So I think I need to cut it back just a little bit. [chuckling]
Dr. Nick: (20:30) Yeah, yeah, yeah. I mean, hey, you're just peeing it out. It's still helping you, but you have to keep in mind that your body can be saturated. Sure.
Aaron Hinde: (20:39) Absolutely. Absolutely. Let's talk about the gym. In Italy, we read this morning on Morning Chalk Up that they forced closure of the CrossFit gyms in Italy. I reached out to many of my friends, gym owners here in the US. They're all open and they say they're as busy as they've ever been. So there's really a mixed viewpoint here on what's going on outside of this country and so far in the US. Should people stay at home? Go to the gym? What do you think?
Dr. Nick: (21:11) So I think-- So if we're talking about CrossFitters specifically, here's our problem, my problem included, right? That most CrossFitters hate missing the gym, right? When you're kind of at that place where it's a habit of yours and you don't want to not go. So I think it needs to be clear and communicated with people who are sick in any manner, especially if you have a fever and cough, myalgia, essentially the signs and symptoms that we mentioned earlier, that is absolutely paramount that you not be in the gym. That you stay home, essentially self-isolate, simply to keep others safe. As I mentioned earlier, the people who are hardest hit by this are those who are immunocompromised for whatever reason, and unfortunately, insofar as-- or rather, even though you may know your own comorbidities, you may know what health issues you have, you have no idea what other people in the gym have. So people in the gym may live with type 2 diabetes, for example, and live in a state of persistent immunocompromise. As such, you are absolutely exposing them to literally infection and potentially, the escalation of that. So I think that keeping sick people out of the gym is important. Additionally, in terms of kind of gym owners-- At my gym personally, at my CrossFit gym, we are providing sanitary wipes. This is here in Denver, Colorado, at CrossFit [Andrea?]. They provide sanitary wipes, and the coach, every single hour, when you're done using your equipment, is encouraging people to take the Clorox wipes and wipe down your equipment. And yeah, that's something that I've noticed at least myself in recent times a lot of gym-goers have been doing.
Aaron Hinde: (23:17) So if you're feeling symptomatic stay home, not necessarily just for yourself, but for other people who may be immunocompromised that you don't even know about at the gym. Make sure you wipe down your equipment. Basic stuff, right? Wash your hands. What do you think about hand-washing versus the antibacterial pump stuff?
Dr. Nick: (23:40) Sanitizer?
Aaron Hinde: (23:40) Hand sanitizer, yeah. One way or the other?
Dr. Nick: (23:43) They're both efficacious. I mean, if the hand sanitizer has a high enough level of alcohol - which, I mean, most hand sanitizers that you can buy in the store absolutely do - they're both efficacious. They both work. Hand-washing, if you're going to do that, the minimum recommended time is 20 seconds. This'll probably be a little bit nerdy, but kind of going through med school and scrubbing and going into surgeries, it's commonly stated that you want to get under your fingernails. And kind of the best way to do that as you're washing your hands is to do something like this: with the soap and the water and your hands, with all your fingernails, essentially, make sure to lather it and wash well. But yeah, the other things that you mention are absolutely recommended. At this point, I would not recommend that anybody cough into their hands or sneeze into their hands; I would recommend rather that you cough into your elbow and essentially-- if you do have to cough into your hands or sneeze into your hands, then make sure that you wash your hands immediately afterward. If you do need to-- I remember just the other day-- This literally happened the other day, Aaron: I was at CrossFit, and the workout had-- It was a barbell workout, so I needed to tape my thumbs, so I tape my thumbs, and just before 3, 2, 1, Go, I felt an eyelash in my eye. So I literally ran to the bathroom, took off the tape on my thumbs, washed my hands. Only after I washed my hands did I stick my finger in my eye, get rid of the eyelash - because I'm not doing a workout like that - and then proceed to join the class again. So you can absolutely touch your nose, touch your mouth, touch your eyes, if you feel that you need to. But do not do so before washing first.
Aaron Hinde: (25:39) Yeah, no, great piece of advice. So solid question back to the vitamin C: any recommendation on dosage, how much vitamin C per day?
Dr. Nick: (25:49) Yeah, so the specific study that I referenced earlier looked specifically at dosages of 200 milligrams and above, so at the bare minimum, that's what I recommend.
Aaron Hinde: (26:03) Great. Have you changed your own travel habits, or what would you recommend people that have travel schedules--?
Dr. Nick: (26:12) So essentially, listen: if people absolutely feel that they need to travel, then travel. But ultimately, I would recommend that people do not-- There are a couple places that are absolutely recommended against at this point, and that's China; that's Iran, Italy, Japan, South Korea. And essentially, absolutely avoid those areas. But if it's, for whatever, reason, absolutely mandated, do so. If you have to do so, I would absolutely recommend avoiding close contact with anyone whom that you are aware has a fever and a cough or other respiratory symptoms.
Aaron Hinde: (26:59) Gotcha. Gotcha. Now, I read that this particular virus has an R0 of two to three, and R0 basically means, when you're infected, how many people would you be expected to infect, right? So if I was infected, then two to three other people would be infected as a result of me. I haven't done the math or looked at any of the math, but it seems like that could spread fairly quickly. And again, we've already stated, fortunately, most people will be minimally symptomatic if not asymptomatic. At what point do we reach herd immunity? Could you talk to herd immunity at all and what that means and at what point does this kind of become like the common cold, where, okay, you might get it on a seasonal basis, but it's not that big of a deal?
Dr. Nick: (27:54) Aaron, I have to apologize: I just got a call and this got interrupted. So I need to pick up the question part of that. Would you say the question again?
Aaron Hinde: (28:01) Yeah, so I was talking about, as it spreads - and we'll continue to see an uptick in cases because of the R0 being two to three - we're going to reach a certain saturation point or something around herd immunity. I've read somewhere, potentially around 60%. After that happens, any estimate on how quickly that could happen, and then what happens after that? We get symptoms; we've been exposed to this virus. Will those symptoms just kind of run their course typically? Or is this something that we need to be concerned about every year now?
Dr. Nick: (28:40) So essentially, that R0 that you mentioned? That's not what I've heard. There's still-- Like I said, right? This is a fast-moving story. As such, I do think it pays to be receptive to the CDC and information that's coming out from the governing health bodies. But essentially, as of right now, from what I've heard, COVID-19 R0 is approximately-- is anywhere from one to three. And that kind of changes, right? Depending on how many people are infected, both symptomatically and asymptomatically. Measles' R0-- Measles is essentially one of the most virulent infections that anyone can get, and the R0 for Measles is 15 to 20.
Aaron Hinde: (29:31) Oh, wow. Okay.
Dr. Nick: (29:32) Yes, right? So just keep that in mind.
Aaron Hinde: (29:33) In perspective, yeah.
Dr. Nick: (29:35) Absolutely. Absolutely. The R0s for influenza? Now that, we know for absolute certain, right? And that is 1.3. So given what I stated earlier, that the R0 of COVID-19 is between one to three, arguably, this could either be less infectious or more infectious than influenza. But it is absolutely not as infectious as other things such as Measles.
Aaron Hinde: (30:01) Good. That's very helpful, put in perspective. Anything else that we haven't covered that you think that the public needs to know regarding Coronavirus?
Dr. Nick: (30:13) No, other than that-- I think that it's obvious that this puts infection at the forefront of everybody's thoughts. But I think what is important to realize and important to know is that there are many other-- As I stated earlier, there are many other variants of Coronavirus, as well as rhinovirus as well as adenovirus as well as everything that kind of causes common infection that is spread to society commonly. The things that are notable that most healthcare practitioners are saying, the simple things: wash your hands; keep your hands away from your mouth, from your nose, from your eyes; cough into your elbow; stay out of work; stay out of the gym if you're sick; all of those things are-- these are-- if you kind of step back and look at them, they're basic. They're very basic. But they are very effective, right? And unfortunately, people, because they're so basic, tend to be dismissive of them, when in reality, they are--
Aaron Hinde: (31:25) Most effective.
Dr. Nick: (31:25) The most effective, yeah. They're step one. So I would just recommend that everybody kind of keep basic sanitary protocols in mind, and yeah, that's pretty much it.
Aaron Hinde: (31:36) Doc, last question, and again, really appreciate your time today. Why do you think this particular virus has gotten so much media attention and hysteria?
Dr. Nick: (31:48) Because it's new and because it's unknown and because it's novel as I stated earlier. When something is entirely novel, when you have any novel coronavirus like MERS, like COVID-19, like SARS, you essentially-- if something is novel, there is no immunity to it on a population scale, right? And as such, it can-- depending on the R0s, it can be very virulent or it cannot be virulent. But essentially, I understand there's a lot of fear. I think what I don't agree with on a fundamental basis is that there's a-- It seems that there's not a lot of evidence-based knowledge being perpetuated and spread about it, or spread on it rather. So a source that I always recommend is the CDC and the CDC website. Anyone can go there, not just doctors. But it is absolutely a great source for information, one, a source of information that is without the hysteria and anxiety that we are commonly seeing these days on television and elsewhere.
Aaron Hinde: (33:08) So avoid the news; go to CDC's website for the latest and greatest; wash your hands; be smart; don't transmit this thing around; stay home if you've got any symptoms going on whatsoever. Doc, really appreciate your time. Doctor Nick from SteadyMD, where can people find out more if-- Quickly tell us what is SteadyMD, and if we wanted to engage your services, how could we do so?
Dr. Nick: (33:34) So SteadyMD is a novel - here we go - is a novel service that has-- started many years back, way before my time with them. But it essentially advocates for a personal relationship with your physician as opposed to going to the doctor like so many of us do these days, and either, A, having a different doctor every single time you come, or B, having your doctor rush you with your appointments despite the fact that you just waited 30 days or even more to see the doctor, and you probably have a lot of built-up anxiety about whatever you're coming in for, and you only-- You get into the room with the doctor and they seem to be rushing you in a five or ten-minute appointment. So SteadyMD gets rid of that by being membership-based. You pay a small fee monthly, and then you can get in contact with your doctor however many times you want with no copays, no waits. You message your doctor; you call us; you video chat us; whatever you'd like, and we're there for you, to attend to kind of whatever your medical needs as well as preventative. I've probably given [inaudible] my mindset towards the lifestyle changes. I am very big on the preventative side of medicine and preventing the diseases of kind of lifestyle, of chronic metabolic diseases that unfortunately is prevalent in society. So yeah, that's what SteadyMD is all about. You can check it out and read more about SteadyMD at www.steadymd.com. And there's a frequently asked questions page that will answer a good amount of people's questions.
Aaron Hinde: (35:26) Awesome. Well, check out SteadyMD, connect with Doctor Nick at @thefittestdoc on Instagram. I am Aaron Hinde, president and cofounder here at LIFEAID Beverage company, with FITAID. Thank you all for your time. Doc, thanks a lot for setting the record straight here. Appreciate it. Take care.
Dr. Nick: (35:44) Yep, take care.
[outro music]








